Fibrocytes boost lung tumor development
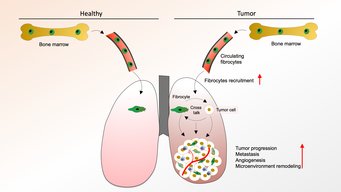
Fibrocyte driven changes to lung tissue remodeling promote tumor growth and metastasis
Fibrocytes are bone marrow-derived cells that have been shown to be important for wound healing. Yet, another role of fibrocytes has now been identified by scientists from the German Center for Lung Research (DZL), working at the Institute for Heart and Lung Research in Bad Nauheim and the Justus-Liebig University in Giessen: in the lung, fibrocytes act on various cell types to promote the growth of lung tumors and the development of metastases. On the molecular level, fibrocytes upregulate the messenger compound endothelin and its two receptors. How these findings can be exploited for the development of new therapeutics is subject of further studies.
Lung cancer is by far the leading cause of cancer death and one of the deadliest diseases worldwide. Lung tumors are frequently diagnosed at an advanced stage, which means the outlook for survival is poor. In fact, this adds to the issue that there are still many gaps in our understanding of the development of lung tumors.
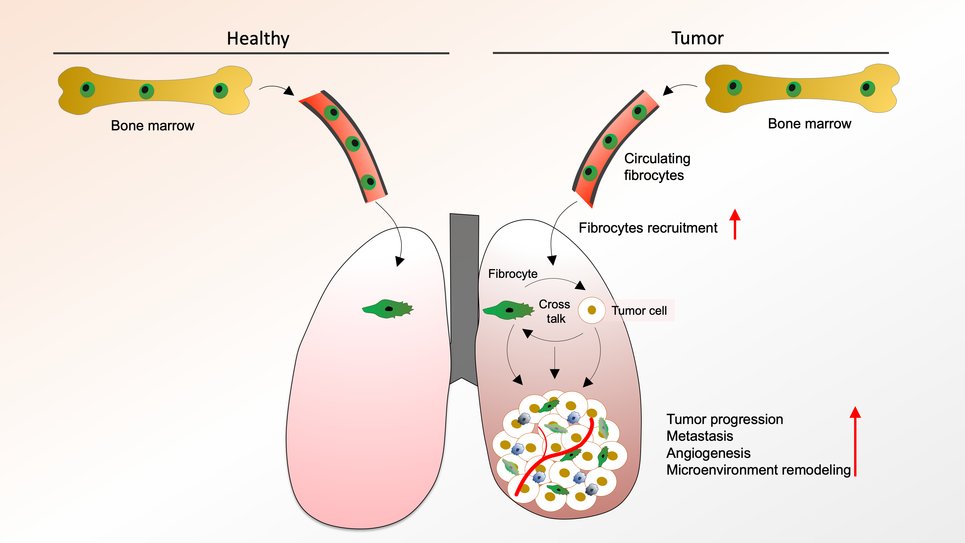
Bone marrow-derived connective tissue cells, so called fibrocytes, migrate into tissues via the blood stream and they have been shown to interact with several other tissue cell types. Fibrocytes that mature into fibroblasts in various tissues are primarily involved in wound healing. In contrast to this known role of fibrocytes, DZL-scientists working in the Department Lung Development and Remodelling at the Max-Planck Institute for Heart and Lung Research and the Justus-Liebig University have now identified a new fibrocyte driven mechanism that regulates the growth of lung tumors in a mouse model.
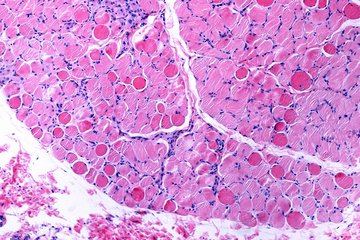
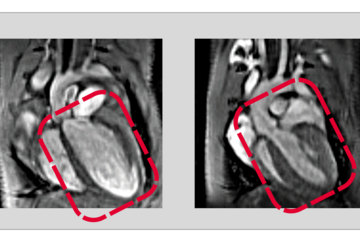
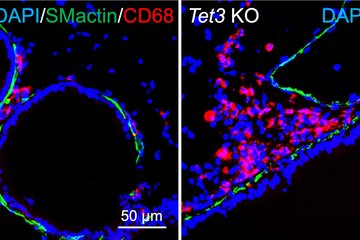
The scientists used mouse lung tumor models to study the effect of selective fibrocyte depletion on the tumor. “We could show that tumors remained much smaller compared to a control group and we also observed fewer metastases”, explains Rajkumar Savai, who led the project. On a cellular level, the number of tumor promoting cells was reduced, which explained the smaller size of tumors. In addition, there were fewer blood vessels surrounding the tumors. Savai adds that “the observation of fewer fibrocytes and macrophages in the tissue surrounding the lung tumor added one more piece to the jigsaw”.
To study the potential clinical relevance of these findings, the Max Planck scientists looked for fibrocytes in tumor tissues of patients suffering from different types of lung cancer. Independent of lung cancer type, the number of fibrocytes was higher in tumor tissue samples compared with healthy control samples. “The more fibrocytes accumulated in the tissue and the higher the number of fibrocytes circulating in the blood, the shorter the disease-free and overall survival of patients”, summarizes Savai.
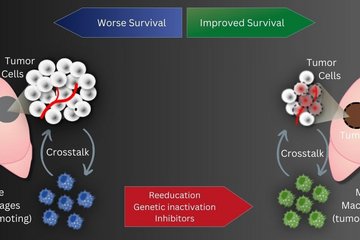
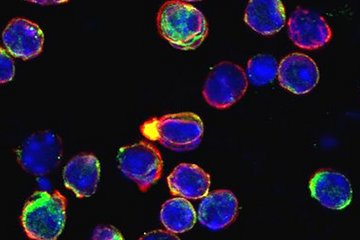
But which mechanisms can explain these findings? In further experiments, the Savai lab was able to demonstrate that fibrocytes act on the tumor microenvironment in a way that facilitates and promotes tumor growth. Fibrocytes interact with cancer cells, suppress the activity of macrophages (white blood cell of the immune system), and support the formation of blood vessels. This cell-to-cell communication is mediated by endothelin-1, a messenger compound secreted by fibrocytes. Cell culture experiments for which fibrocytes were co-cultured with tumor cells and blood vessel derived endothelial cells, showed an increased production of endothelin-1 and an increase in endothelin receptors on tumor cells. “In contrast, the blockade of endothelin-1 receptors in both cell culture and mouse model experiments led to a suppression of fibrocyte-associated tumor-promoting effects”, explains Savai.
The results of this study underline the clinical relevance: “It has been discussed for quite a while whether fibrocytes can serve as a biomarker for the prognosis of lung tumor development after surgery. Our data supports this idea,” says co-author Werner Seeger, head of the department. If further studies confirm the blockade of the endothelin-receptor as a therapeutic concept, this may lead to the development of new targeted medications.