Re-programmed macrophages fighting against lung cancer
Often lung cancer ends fatally. A major reason for this is that the tumour frequently is being detected at an advanced stage only. Furthermore, the effectiveness of modern therapies, such as the immune therapy, is limited as well. Scientists of the Max Planck Institute for Heart and Lung Research in Bad Nauheim and the Justus Liebig University in Giessen proved that a certain group of leukocytes, so-called tumour-associated macrophages, play an essential role during the formation of metastases. The hereby involved molecular regulatory cascade might be a target for future therapeutic measures.
Lung cancer probably leads to the highest number of deaths among tumour diseases. The fact that the disease is mostly fatal – only 14 percent of the patients are surviving the first five years after diagnosis – originates from deficits to detect it at an early stage and missing effective therapies at advanced stages.
Hence the currently applied immune therapy is only partly successful or the curative effects diminish in the course of the treatment. Scientists of the Department “Lung Development and Remodelling” at the Max Planck Institute for Heart and Lung Research in Bad Nauheim have, together with colleagues of the Justus Liebig University in Giessen, identified an approach for a new immune therapeutic treatment of lung cancer.
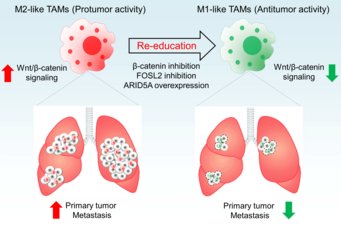
Leukocytes play an important role in fighting against many diseases. Often these cells succeed in preventing the formation of a tumour. Investigating the cellular background of thistumour defense was the aim of the scientists: “We are examining the entire spectrum of the cells and chemical messengers in the environment of tumours, such as surrounding blood vessels, immune cells, fibroblasts, signalling molecules and the extra-cellular matrix. In this course we discovered that a certain group of macrophages appeared in large numbers”, explained Project Leader Rajkumar Savai. Tumour-associated macrophages (TAMs) contribute significantly to the development of inflammations in the tumour’s environment. The scientists identified that a high number of these cells correlates with a bad diagnosis of the patients. “Initially the result was surprising for us as the TAMs usually impede the cancer. However, we could see that some variants of these cells stimulate tumours”, Savai said.
In the further course of the study the Max Planck Scientists found out how macrophages that inhibited tumours evolved to those that promoted them. Accordingly, the key molecule is ß-Catenin, a protein active in diverse regulatory chains. “This protein activates the expression of certain genes at the level of transcription”, Savai explained. Intervening at this position of the signal way might therefore help decreasing a re-programming from tumour-inhibiting TAMs to tumour-supporting TAMs. “By this means a promising therapeutic approach can be established. With the discovery of this molecular switch we make an important step towards a novel approach in the precision medicine”, said Werner Seeger, Director at the Max Planck Institute and the Medical Clinic II of the Justus Liebig University. Following these findings, the tumour-inhibiting behaviour of macrophages in the environment of lung tumours can be supported selectively and at the same time side effects in other organs can be avoided.
MH, UNI GI